Disc Herniation Treatment in Dublin

At our Dublin-based clinic, we offer comprehensive disc herniation treatment to help patients regain their mobility and find relief from the debilitating pain caused by this condition. Our team of dedicated experts is committed to providing personalized care and employing advanced therapies to address your specific needs.
We understand that each patient's condition is unique, and that's why we offer personalized treatment options to ensure the best possible outcomes.
Our experienced professionals will conduct a thorough evaluation, including a comprehensive medical history review and diagnostic imaging, to accurately diagnose your disc herniation. Based on this assessment, we will develop a customized treatment plan tailored to your individual needs.
In many cases, disc herniation can be effectively managed without the need for surgery.
Our clinic specializes in a range of non-surgical interventions that aim to alleviate pain, reduce inflammation, and facilitate healing. These may include physiotherapy, non surgical spinal decompression therapy, and pain management techniques. Our team will work closely with you to determine the most appropriate non-surgical approach based on your specific condition and preferences.https://dcphysiotherapy.ie/non-surgical-spinal-decompression/
This is a common lower back disorder. Lumbar Disc Herniation is one of the most common diseases that produces lower back pain and/or leg pain in adults.
A herniated disc is a displacement of disc material (nucleus pulposus or annulus fibrosis) beyond the intervertebral disc space.
This herniation process begins from failure in the innermost annulus rings and progresses radially outward.
The damage to the annulus of the disc appears to be associated with fully flexing the spine for a repeated or prolonged period of time.
The nucleus loses its hydrostatic pressure and the annulus bulges outward during disc compression. Other names used to describe this type of pathology are: prolapsed disc, slipped disc or spinal disc herniation, herniated nucleus pulposus and disc protrusion.
We believe in a comprehensive approach to healing, focusing not only on treating the immediate symptoms but also on long-term recovery and prevention of future complications.
Our team will provide you with guidance on lifestyle modifications, exercises, and ergonomic practices to strengthen your back, improve posture, and reduce the risk of recurrent disc herniation. We are committed to supporting you throughout your journey toward improved spinal health and overall well-being.

It is a medical condition affecting the spine, in which a tear in the outer fibrous ring of IV disc allows the soft central portion to bulge out beyond the damaged outer ring. This condition occurs when the soft centre of a spinal disc pushes the disc through a crack in the tougher exterior casing. It occurs rarely in children, and it is most common in young and middle-aged adults. A herniation may develop suddenly or more gradually over weeks or months.
- The management of disc herniation requires an interprofessional team. The initial treatment should be conservative, unless a patient has a severe neurological compromise.
- Surgery is usually the last resort as it does not always result in predictable results. Patients are often left with residual pain and neurological deficits, which are often worse after surgery.
- Physical therapy is the key for most patients. The outcomes depend on many factors, however, those who participate in regular exercise and maintain a healthy body weight tend to have better outcomes than those who have a more sedentary lifestyle.
- The management of disc herniation requires an interprofessional team. The initial treatment should be conservative, unless a patient has a severe neurological compromise.
- Surgery is usually the last resort as it does not always result in predictable results. Patients are often left with residual pain and neurological deficits, which are often worse after surgery.
- Physical therapy is the key for most patients. The outcomes depend on many factors, however, those who participate in regular exercise and maintain a healthy body weight tend to have better outcomes than those who have a more sedentary lifestyle.
Types Of Herniations
Physiotherapy Management -Disc Herniation Treatment in Dublin
Physical therapy often plays a major role in herniated disc recovery. It involves the below key actions:
- Ambulation and resumption of exercise
- Pain control
- Education re maintaining healthy weight
Physical therapy programmes are often recommended for the treatment of pain and restoration of functional and neurological deficits associated with symptomatic disc herniation.
Physical therapy is preferred to passive modalities. There are a number of exercise programmes for the treatment of symptomatic disc herniation e.g.:
- Aerobic activity (eg, walking, cycling)
- Directional preference (McKenzie approach)
- Flexibility exercises (eg, yoga and stretching)
- Proprioception/coordination/balance (medicine ball and wobble/tilt board)
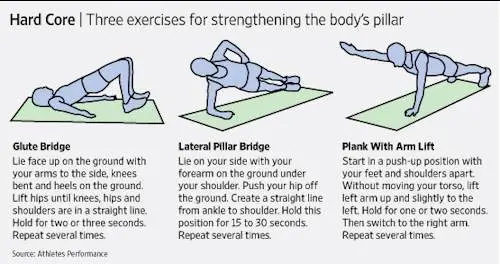
- Strengthening exercises
- Motor control exercises (MCEs)
MCES (Stabilisation / Core Stability Exercises)
They are a common type of therapeutic exercise prescribed for patients with symptomatic disc herniation.
- Designed to re-educate the co-activation pattern of abdominals, paraspinals, gluteals, pelvic floor musculature and diaphragm.
- The biological rationale for MCEs is primarily based on the idea that the stability and control of the spine are altered in patients with LBP.
- Programme begins with recognition of the natural position of the spine (mid-range between lumbar flexion and extension range of motion), considered to be the position of balance and power for improving performance in various sports.
- Initial low-level sustained isometric contraction of trunk-stabilising musculature and their progressive integration into functional tasks is the requirement of MCEs.
- MCE is usually delivered in 1:1 supervised treatment sessions and sometimes includes palpation, ultrasound imaging and/or the use of pressure biofeedback units to provide feedback on the activation of trunk musculature.
- A core stability program decreases pain level, improves functional status, increases health-related quality of life and static endurance of trunk muscles in lumbar disc herniation patients. Individual high-quality trials found moderate evidence that stabilisation exercises are more effective than no treatment.
Different studies have shown that a combination of different techniques will form the optimal treatment for a herniated disc. Exercise and ergonomic programs should be considered as very important components of this combined therapy.
General Rules For Exercise / Do And Don'ts
- Do exercise slowly. Hold exercise position for slow count of 5. Start with 5 repetitions and work up to 10. Relax completely between the repetitions.
- Do exercise for 10 min twice a day.
- Care should be taken while doing exercise which can be painful.
- Exercise daily without fail.
A herniated disk, which can occur in any part of the spine, can irritate a nearby nerve. Depending on where the herniated disk is, it can result in pain, numbness or weakness in an arm or leg.
Many people have no symptoms from a herniated disk. Surgery is usually not necessary to relieve the problem.
Symptoms
Most herniated disks occur in the lower back, although they can also occur in the neck. Signs and symptoms depend on where the disk is situated and whether the disk is pressing on a nerve. They usually affect one side of the body.
When To See A Doctor?
Seek medical attention if your neck or back pain travels down your arm or leg, or if you also have numbness, tingling or weakness.
Risk Factors
Complications
Just above your waist, your spinal cord ends. What continues through the spinal canal is a group of long nerve roots that resemble a horse’s tail (cauda equina).
Rarely, disk herniation can compress the entire spinal canal, including all the nerves of the cauda equina. Rarely, emergency surgery might be required to avoid permanent weakness or paralysis.
Seek emergency medical attention if you have:
Prevention
To help prevent a herniated disk, do the following:
What's The Difference Between A Bulging Disk And A Herniated Disk?
Answer From Randy A. Shelerud, M.D.
Disks act as cushions between the vertebrae in your spine. They’re composed of an outer layer of tough cartilage that surrounds softer cartilage in the center. It may help to think of them as miniature jelly doughnuts, exactly the right size to fit between your vertebrae.
Disks show signs of wear and tear with age. Over time, disks dehydrate and their cartilage stiffens. These changes can cause the outer layer of the disk to bulge out fairly evenly all the way around its circumference — so it looks a little like a hamburger that’s too big for its bun.
A bulging disk doesn’t always affect the entire perimeter of a disk, but at least a quarter if not half of the disk’s circumference is usually affected. Only the outer layer of tough cartilage is involved.
A herniated disk, on the other hand, results when a crack in the tough outer layer of cartilage allows some of the softer inner cartilage to protrude out of the disk. Herniated disks are also called ruptured disks or slipped disks, although the whole disk does not rupture or slip. Only the small area of the crack is affected.
Compared with a bulging disk, a herniated disk is more likely to cause pain because it generally protrudes farther and is more likely to irritate nerve roots. The irritation can be from compression of the nerve or, much more commonly, the herniation causes a painful inflammation of the nerve root.
If an imaging test indicates that you have a herniated disk, that disk might not be the cause of your back pain. Many people have MRI evidence of herniated disks and have no back pain at all.

